Human papillomavirus (HPV) – Science Notes
Papillomavirus is a combination of papillomavirus (PA), polyomavirus (PO), and vacuolating agent (VA). The name “papova” comes from “papillae,” which refers to a lump, growth, or pimple, and “oma,” which means tumor. Historically, these viruses have been classified into families Papovaviridaebut this classification is no longer recognized. These viruses are now divided into two distinct families: human papillomavirus (HPV) and human polyomavirus.
- Papilloviridae: Human papillomavirus (HPV) family
- Polyomaviridae: Human polyomavirus family
Cavitation agents are also classified as Polyomaviridae A family is a group of viruses that share certain characteristics. Papillomavirus and polyomavirus are both DNA viruses. naked viruswhich means they are missing envelopes. This property makes them more stable in the environment and easier to spread through direct or indirect contact.
Human papillomavirus (HPV)
human papillomavirus (HPV) is a group of more than 200 related viruses that primarily infect skin and mucous membranes, such as the genitals, mouth, and throat. HPV infection occurs in epidermal cell division or basal layer cells The virus enters skin cells and begins to replicate. HPV is Highly host specific and tissue specificitymeaning it typically infects one species and targets a specific type of tissue.
One of the challenges in studying HPV is that it cannot be cultured under laboratory conditions. it Grows only in proliferating stratified squamous epithelial cellsthey are difficult to grow in vitro. This means that traditional cell culture methods for isolating the virus are not suitable for HPV. at last, detect Detection of HPV infection relies on other techniques, e.g. Immunoassay and gene probe.
HPV test
Because HPV cannot be cultured, testing focuses on identifying the viral genetic material in infected cells. This can be done by something like DNA hybridization (PCR, Southern blot hybridization) or in situ hybridization. Mucosal smear (for example, from the cervix, vagina, or anus) is usually used for testing, and Pap smear test It is often combined with HPV testing to detect the presence of HPV and identify specific strains of the virus.
One notable limitation is that, so far, There are no tests available to detect HPV in male samples. However, there is good evidence that men can develop Condyloma acuminata Due to HPV infection, although the occurrence of cancer is rare compared to women. Men are considered mediums HPV transmission, including person-to-person transmission Women who have sex with women (WSW).
Types of human papillomavirus HPV virus
HPV types are classified according to their organizational orientationor a preference for infecting certain types of tissue. HPV types are divided into two broad categories:
- skin type: These mainly infect the skin and cause common warts.
- Mucosal type: These can infect mucous membranes and are associated with genitals warts, and cervical cancer.
In mucosal types, more than 40 HPV types are sexually transmitted, these are designated genital type. These types are further classified based on their association with: reproductive tract cancer as:
- high risk type:HPVs 16, 18, 31, 33, 45, 56, 58, 59, and 68 are associated with an increased risk of: cervical cancer and other cancers.
- low risk type:HPV 6 and 11 are mainly responsible for Condyloma acuminata Usually does not cause cancer.
- Medium risk type: These types are associated with low-risk precancerous lesions but are not as associated with cancer as high-risk types.
Cervical Cancer and HPV
One of the most important medical issues related to HPV is its association with cervical cancer. cervical cancer It is the third most common cancer among women worldwide, second only to Chest and colorectal cancer. Mainly caused by high-risk HPV infection, especially HPV 16 and 18they are responsible for approximately 98% of cervical cancers.
In fact, the end 50% women Internal infection with genital HPV 2 years become sexually active, it is estimated 80% of women will be infected with HPV during their lifetime. However, most infections are transient and asymptomatic, and the body’s immune system clears the virus without any long-term effects. In some cases, especially high-risk HPV types, the infection persists and may lead to Cervical intraepithelial neoplasia (CIN)which is a precursor to cancer.
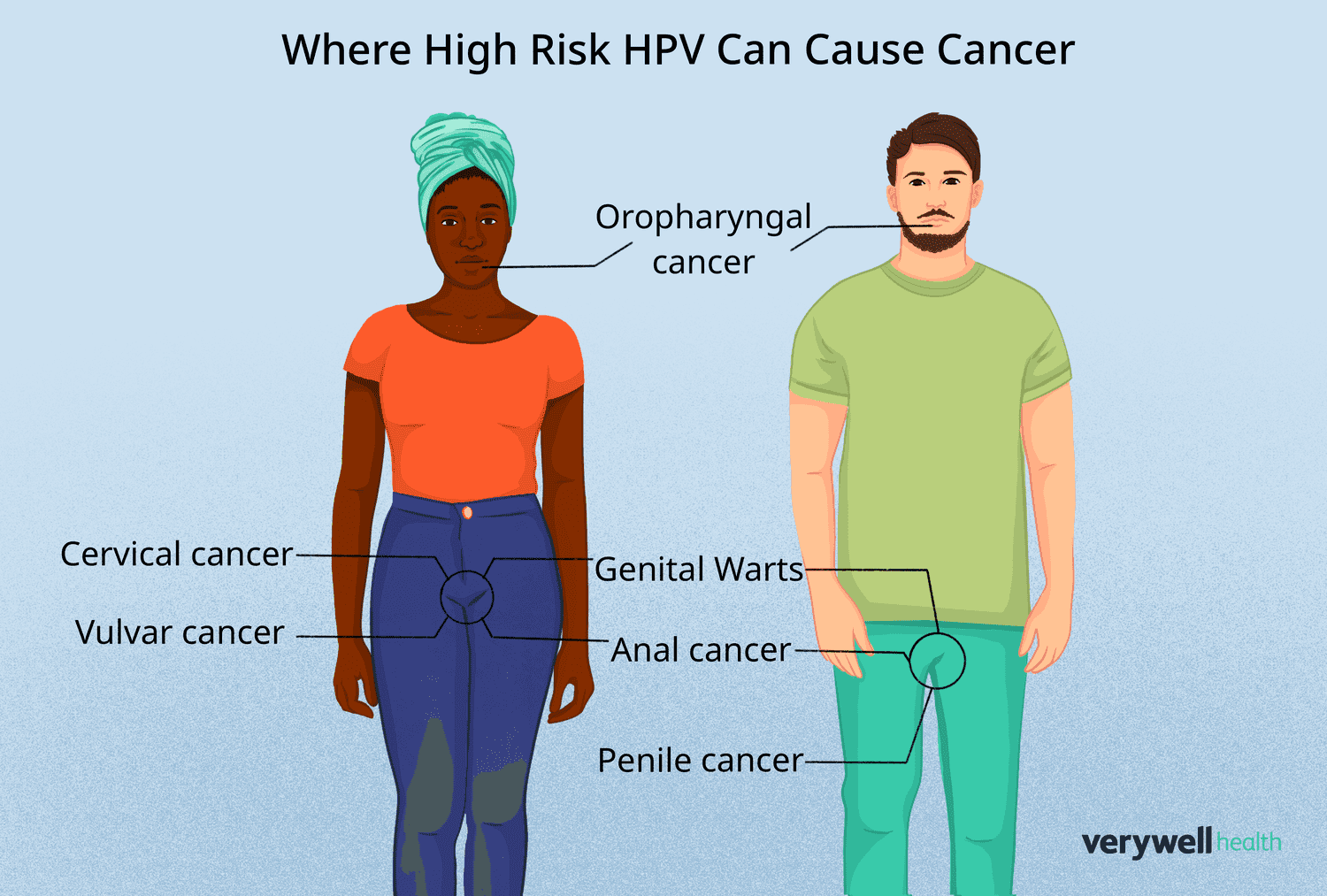
HPV and other cancers
although cervical cancer HPV is the most well-known cancer associated with HPV, but other cancers are also linked to the virus. anal cancer Becoming increasingly common, especially among men who have sex with men (gay men) and people living with HIV. Although anal cancer is still less common than cervical cancer, its incidence is increasing.
HPV can also cause cancer Oropharynx,include throat, tonsiland Tongueespecially for people who perform oral sex. Research shows that more and more Oral and vaginal sex partnerslack Use a condomand poor dental hygiene Associated with a higher risk of HPV-related oropharyngeal cancer.
Cervical Cancer Risk Factors
Some risk factors are associated with human papillomavirus Infect and the subsequent development of cervical cancer. These include:
- Number of sexual partners: Women who have multiple sexual partners are at higher risk of contracting HPV.
- age of first intercourse: Starting sexual activity too early increases the risk of HPV exposure.
- Male partner’s sexual activity: Male partners who have multiple sexual partners may increase the risk of HPV transmission.
- Failure to use barrier contraception: Not using condoms increases the likelihood of HPV transmission.
- smoking: Smoking weakens the immune system and increases susceptibility to persistent HPV infection.
- Oral contraceptive use: Long-term use of birth control pills may increase the risk of cervical cancer, especially in women who smoke.
- multiple pregnancy: Women who have had multiple pregnancies may have a higher risk of cervical cancer.
- Immunosuppression: Individuals with weakened immune systems (such as those with HIV) are more likely to develop persistent HPV infection.
HPV diagnosis
Diagnosis of HPV Infections often involve a combination of methods:
- Biopsy and histology: A biopsy sample of abnormal tissue is examined to identify changes characteristic of HPV infection.
- Pap smear: This is a widely used screening tool that involves collecting cells from the cervix. If HPV is suspected, additional testing may be required, e.g. DNA testing (PCR, Southern blot hybridization) or in situ hybridization Can proceed.
Benign lesions caused by HPV
Many types of HPV infection can cause benign lesions It does not cause cancer but may be uncomfortable or cause cosmetic problems. These include:
- Common warts (Wart vulgaris): Characterized by a rough, raised surface, common on the hands, knees, and feet.
- Flat warts (Flat warts): Smoother and flatter than regular warts, usually seen in children.
- butcher’s wart: Related to butchers, but the reason for their appearance in this profession is not entirely clear.
- Condyloma acuminata Genital warts (genital warts): Caused by HPV types 6 and 11, these warts appear in the genital and anal areas. They are usually benign but can be uncomfortable and cause complications during delivery.
Malignant or potentially malignant lesions
HPV may also cause Malignant or potentially malignant lesionsinclude:
- Bowenoid papulosis: Multiple pimple-like rashes appear on the penis or vulva Bowen’s disease. These lesions may eventually become malignant.
- intraepithelial dysplasia: Abnormal changes in the cervical epithelium, often called CIN (cervical intraepithelial neoplasia), vanity (vaginal intraepithelial neoplasia), and Frame number (Vulvar intraepithelial neoplasia). The most severe form of dysplasia, CIN 3, involves all layers of the epithelium and has a high likelihood of progression to invasive cancer.
Vaccination and prevention
The best way to prevent HPV-related diseases is to Vaccination. The HPV vaccine is most effective when given before sexual activity begins. this Department of Disease Control The recommended age for HPV vaccination is between 11-12th (Although vaccinations can begin at age 9). one 3 dose regimen Typically used:
- first dose: Given at first appointment.
- second dose: 1-2 months after the first dose.
- third dose: 2 months after the second dose.
Available vaccines include:
- 2vHPV (Cervarix): Targets HPV 16 and 18 (approved for use in women only).
- 4vHPV (plus vaccine): Targets HPV types 6, 11, 16 and 18 (approved for use in men and women).
- 9vHPV (GV-9): Targets 9 HPV types (6, 11, 16, 18, 31, 33, 45, 52 and 58) and can be used by both men and women.
These vaccines are preventivemeaning they can prevent infection but cannot treat existing infections.
Treatment and Management
Currently, no antiviral drugs Can be used to treat HPV infection. Vaccines can prevent Precancerous lesions and non-invasive cancers, such as cervical precancerous lesions, but they do not cure active infections. HPV-related treatments wart Lesions typically include topical treatment, cryotherapy, or surgical excision.
in conclusion
Human papillomavirus (HPV) infection is a global public health problem and has a significant impact on the development of cancers such as cervical cancer. Although there is no cure for existing HPV infections, you can take the following preventive measures Vaccination It has been shown to reduce the incidence of HPV-related cancers. Comprehensive education, early detection, and vaccination are critical to reducing the public health burden of HPV.


